A recent retrospective study [1] conducted by researchers at University Hospital Tuebingen focused on identifying imaging and clinical predictors of overall survival and treatment response in patients with metastatic melanoma undergoing immunotherapy.
Advances in immunotherapy have improved the prognosis for metastatic melanoma patients. However, resistance against immune checkpoint inhibitors and other types of immunotherapy occurs in more than half of the patients.
“Therefore, identification of baseline response and survival predictors in these patients is crucial and could help to stratify patients for the right therapy choice,” Dr. Othman explained. “To our knowledge, the present study is the first to investigate imaging biomarkers solely extracted from baseline CT imaging in a representative patient cohort with metastatic melanoma undergoing immunotherapy, which is the therapy of choice at present.”
103 patients were retrospectively selected and randomly assigned to training (n=69) and validation cohort (n=34). Clinical and imaging biomarkers, as well as CT texture features, were extracted from the largest target lesion (RECIST 1.1) at baseline:
- Clinical tumor markers (serum lactate dehydrogenase (LDH) and the low molecular calcium-binding, acidic cytoplasmic protein S100B),
- CT imaging biomarkers (tumor burden and Choi density) and
- CT texture parameters (entropy, kurtosis, skewness, uniformity, mean of positive pixels (MPP), and uniformity of positive pixel distribution (UPP)).
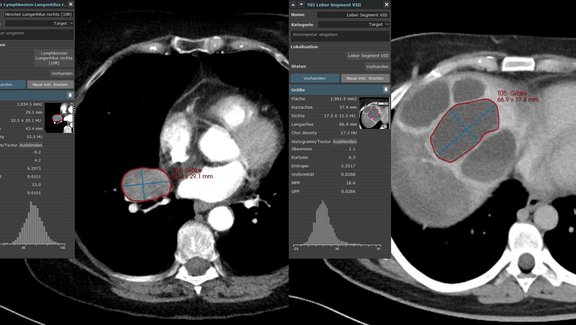
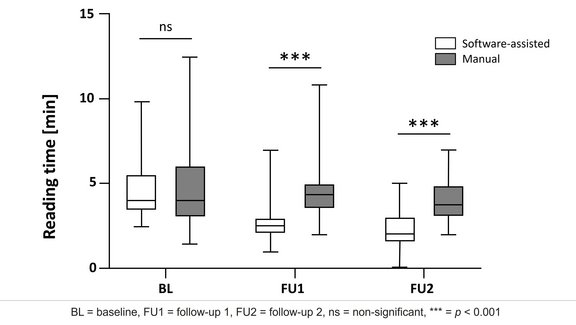
mint Lesion™ was used to extract the CT imaging biomarkers and area-based first-order texture parameters, as well as to assess the treatment response according to RECIST 1.1.
In the training cohort, baseline S100B was confirmed as a clinical predictor for overall survival (OS), with a hazard ratio (HR) of 2.543 in multivariable analysis (p = 0.018). Baseline RECIST 1.1 tumor burden (as sum of the longest diameters of the target lesions) and kurtosis were also identified as independent predictors for OS (HR = 1.657, p = 0.002 and HR = 1.611, p < 0.001). The three predictors were confirmed in the validation cohort (p < 0.048). When combined with baseline S100B levels, tumor burden and kurtosis showed incremental predictive capacity (C-index = 0.720).
S100B was acknowledged as the only predictor of treatment response at first follow-up from all analyzed clinical and imaging parameters (OR = 0.630, p = 0.022).
“We identified independent baseline clinical (S100B) and imaging (tumor burden and kurtosis) predictors in patients with metastatic melanoma undergoing immunotherapy, which when used combined have a good predictive capacity for patient survival,” the authors concluded. Further studies are needed to assess the potential predictive value of higher-order radiomic features.
[1] Schraag A., Klumpp B., Afat S., Nikolaou K., Eigentler T. K., Othman A. E. (2019) Baseline clinical and imaging predictors of treatment response and overall survival of patients with metastatic melanoma undergoing immunotherapy, European Journal of Radiology, https://doi.org/10.1016/j.ejrad.2019.108688