Adenomyosis is a gynecological condition of the uterus and a form of endometriosis. Approximately 10 percent of women of reproductive age are affected by adenomyosis or endometriosis, which corresponds to around 200 million patients worldwide. Currently, there is no reliable method for the early detection of adenomyosis. However, MRI scans can produce standardized 3D images of the pelvis, offering detailed visualization of soft tissues. This technique captures the anatomy of the uterus as well as pathological changes, taking into account the individual menstrual cycle.
As part of the RACOON FADEN project, researchers are conducting a controlled clinical study to investigate radiological characteristics after MRI scans for the early detection of adenomyosis in young patients. The resulting data will be made accessible, while simultaneously building an infrastructure to extract imaging biomarkers of the uterus within the Network University Medicine (NUM), enabling scalable use.
We spoke with the project leaders, Prof. Dr. med. Sylvia Mechsner and Prof. Dr. med. habil. Matthias May, EBIR, to learn more about the project.
Mint Medical: How did the RACOON FADEN project come about?
May: The project came about primarily because we identified a significant gap in the care of young patients with adenomyosis. Professor Mechsner has already done a great deal of preliminary scientific work in this area: the current understanding is that patients diagnosed with endometriosis — the spread of the disease to other organs, which can also lead to infertility — have often been experiencing symptoms for years but were not taken seriously.
Mechsner: That’s why we want to develop an investigator-independent method, an early detection tool that can be used for women with severe menstrual pain. Currently, there is often a diagnostic delay of up to 10 years. Menstrual pain is dismissed as normal, and nothing is visibly wrong. As a result, these complaints are not pursued further, and the affected women are not offered appropriate treatment. Ten years later, issues such as infertility, unbearable pain, or cysts suddenly arise, and the diagnosis of endometriosis is made, even though these women have been suffering for years.
What we lack so far is a closer examination of the uterus itself. FADEN stands for “Early Detection of Adenomyosis” (Früherkennung Adenomyose), and we’ve made it our goal to take a much closer look at the uterus. As gynecologists, we naturally use ultrasound, but when we detect serious changes with it, they are often already irreversible. The key question is: are there really early signs? And that leads to the next question: what does a healthy uterus actually look like? Not every woman who visits a gynecologist for contraception or a cancer screening automatically gets an ultrasound or MRI scan. Therefore, we know very little about what a healthy uterus should actually look like.
Mint Medical: How does endometriosis develop in the first place?
Mechsner: We assume that the disease originates in the uterus – that strong cramps can cause microtraumas between the endometrium and the muscular layer, which activates tissue repair mechanisms. In the process, stem cells might migrate – either into the muscle wall, leading to thickening, or they disrupt and alter the junctional zone. If these stem cells travel through the fallopian tubes into the abdominal cavity, endometriosis can develop there.
Mint Medical: How is the RACOON FADEN study designed?
Mechsner: We first conducted research to determine which cycle-dependent changes of the uterus need to be considered. There is currently very little data available in this area. We decided to examine the uterus once during menstruation and once around ovulation. We are also including young girls aged 13 to 30 in order to capture age-dependent differences. Our focus is on individuals with severe symptoms who come from endometriosis centers. However, we are excluding cases of severe endometriosis, deeply infiltrating endometriosis, and hormone therapies, as these can alter the uterus. We are also excluding women who have been pregnant, as this can also affect the uterus.
A unique aspect of our study, which, to my knowledge, is being conducted worldwide for the first time, is that we are including healthy participants: 104 healthy women and 104 women with symptoms. This is a major advantage of our study, as it has never been investigated before what a truly healthy uterus looks like.
May: MRI is an imaging method that, as long as no contrast medium is used, has virtually no side effects. In this study, it was particularly important to us to choose an approach that achieves high-quality imaging with minimal effort, surpassing the quality of sonographic imaging used so far.
Mint Medical: What are the goals of the FADEN study and what challenges must be overcome in this research?
Mechsner: One of the goals, as mentioned before, is to describe the morphology of a healthy uterus and verify how adenomyosis can be detected and described. We want to particularly investigate which early forms of the disease can be identified. Additionally, we aim to see how findings from gynecological ultrasounds can be correlated with MRI scans, as they are two different methods that visualize different structures. Of course, we also want to relate these findings to the intensity of pain.
I also believe that the asymmetry of the uterine wall—where one side is thicker and the other thinner—can be an early sign. I observe this repeatedly in my patients, and when they take hormones, the asymmetry decreases. To me, this is a clear indication of an early sign. We will be able to observe this much better in MRI, as the imaging is far more precise. This will help us better understand this phenomenon.
May: Exactly, another primary goal of the study is the analysis of the junctional zone in terms of its thickness. With the standardized examination method we’ve now implemented across multiple centers, we aim to identify additional parameters and indicators to determine whether a person is healthy or affected by the disease.
The biggest challenge in the FADEN study is certainly establishing an infrastructure for a diagnostic method that is completely new and doesn’t yet exist in the literature. While researchers have analyzed uterine MRIs in cases of adenomyosis before, it has not been done with a specific protocol nor in a multicentric, prospective approach. This is definitely what’s new about our study.
Mechsner: Another challenge is the organizational aspect of having to account for the menstrual cycle, which means the MRI scans must be planned according to the cycle. This is not always easy, as the MRI machine must be available at the desired time. Additionally, the uterus is a muscle, and we want to keep the examination as simple as possible—without using contrast agents or administering spasmolytics.
Mint Medical: To what extent is the existing RACOON infrastructure being used?
May: We wouldn't be able to conduct this study if the NUM RACOON infrastructure and the NUM-NUKLEUS didn't already exist. We are utilizing all components of the RACOON infrastructure: The data management and structured reporting provided by Mint Medical play an essential role. A standout feature of mint Lesion™ is its ability to precisely measure tissue thickness, with standardized measurements consistently tracked across multiple time points. This allows me to precisely track where and at what point in the menstrual cycle the measurement in the preliminary examination was taken and how to reproduce that examination. All collected data is recorded and evaluated in a structured reporting template.
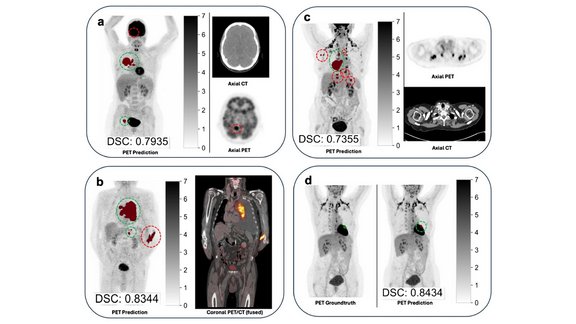
For volumetric segmentation, we use the SATORI platform from Fraunhofer MEVIS. We developed a completely new workflow for this unique examination technique – a method the platform had not seen before. Several adjustments had to be made, and we received strong support in this process.
Once all volumetric segmentations in our study are complete, we will train a neural network. Our goal is to analyze future data within this infrastructure with minimal manual interaction or the need for corrections. There will always be a final revision step by a physician who will review, confirm, or potentially modify the results before the data can be used for study purposes. However, the majority of the workload should eventually be as automated as possible.
One challenge with the scans is the movement of the uterus and intestines within the pelvis, which needs to be compensated for. This is where our third infrastructure partner comes in: the Joint Imaging Platform (JIP) of the German Cancer Center DKFZ. The Joint Imaging Platform at DKFZ has already developed a program that transfers volumetric segmentations from the anatomical sequence – where the junctional zone is particularly visible – to other datasets for tissue characterization. This enables us to evaluate different zones of the uterus separately, even if they aren’t clearly distinguishable in the raw imaging. This way, we can ensure the volumetric transfer across multiple time points, even with possible shifts.
So, I’d like to give a big shout-out to our three technical partners. The collaboration here has been truly intense and effective.
Mint Medical: What role does artificial intelligence play in the project?
May: The role of artificial intelligence in this project lies in utilizing the collected data to train an AI system. The goal is to develop a platform by the end of the project that can accelerate or support research on women’s health, particularly regarding the adenomyosis-endometriosis complex, within the German university medical system.
In principle, this examination technique of the uterus could also be adapted or scaled for other oncological diseases. This is a crucial point: the infrastructure we are building should ultimately be applicable not just for one specific condition, but for various uterine diseases as well.
Prof. Dr. med. Sylvia Mechsner is Senior Physician and Head of the Endometriosis Center at Charité in Berlin. She holds the first and only professorship for endometriosis research in Germany. Between 2011 and 2013, Prof. Mechsner received several prestigious awards for her research on endometriosis. She is the coordinator of the FADEN project.
Prof. Dr. med. habil. Matthias Stefan May, EBIR is Senior Consultant and Associate Professor at the Department of Radiology at University Hospital Erlangen. He has extensive experience in clinical training, product development, and research. As the clinical coordinator of the Imaging Science Institute, he leads several innovative research projects and has authored over 100 international publications. Prof. May is also a coordinator of the FADEN project.
The RACOON FADEN project is coordinated by the Department of Gynecology at Charité Berlin and the Department of Radiology at University Hospital Erlangen. The project involves 13 university endometriosis centers, including gynecology and radiology departments, 6 sites of the clinical trial platform NUKLEUS, as well as the German Cancer Research Center (DKFZ) in Heidelberg, Fraunhofer MEVIS Institute in Bremen, and Mint Medical as technical partners within RACOON.
To learn more about the project, check out the website of the Netzwerk Universitätsmedizin (NUM) or the RACOON Network site.