
Structured Reporting and Artificial Intelligence in Prostate Diagnostics: An Interview with Prof. Dr. Thorsten Persigehl
In radiology, structured reporting and artificial intelligence (AI) are no longer visions of the future. Both have the potential to add significant value to patient care and expand diagnostic capabilities. But how do these technologies actually change the day-to-day work of radiologists?
To shed light on the practical implications of these developments, we spoke with Univ.-Prof. Dr. Thorsten Persigehl from University Hospital Cologne. As an expert in oncologic imaging and head of the Radiologic CIO (radCIO), Prof. Persigehl shares his insights on how reports are created with mint Lesion, why structured reporting has become indispensable to him, and how artificial intelligence assists in prostate segmentation and reporting: A practical discussion on efficiency, quality, and the future of prostate diagnostics.
Prof. Persigehl, what does your typical prostate workflow look like?
In our department, clinical prostate MRI reporting is performed in mint Lesion. The images are first opened and manually analyzed in the PACS as usual.
Documentation then takes place in parallel on a separate monitor in mint Lesion, supported by an integrated AI system that automatically segments the prostate volume in advance. By entering the PSA value, the software also automatically calculates the prostate density.
In addition, it is possible to obtain a “second opinion” from another integrated AI system, which suggests potential prostate lesions as a kind of second reader option. Of course, these suggestions must always be reviewed and validated carefully based on one’s own clinical expertise.
If prostate lesions are detected in the mpMRI, they are entered in a structured way within the mint Lesion software. The system assists in assigning the correct PI-RADS classification and anatomical localization. Once the lesion is outlined on the transverse T2-weighted series, this annotation is automatically transferred into the prostate schema. As a result, the mint Lesion report includes both a screenshot of the lesion on the T2-weighted image and a corresponding schematic representation, color-coded according to the PI-RADS risk level for prostate carcinoma.
mint Lesion also enables us to document additional relevant findings easily – such as possible infiltration of the seminal vesicles or adjacent organs, lymph node or bone metastases, and incidental findings like rectal or bladder carcinomas.
What advantages do you see in structured reporting?
Personally, I’m a big advocate of structured reporting in oncologic imaging. Here in Cologne, we have already implemented structured reporting for several tumor entities, such as liver, pancreas, esophagus, and rectum carcinomas.
In our view, structured reporting offers numerous advantages. First and foremost, it ensures that all clinically relevant data are captured systematically and included in the report. This allows us to provide our referring clinicians with precisely the information they need for treatment decisions.
Another major benefit (especially here at University Hospital Cologne) is the impact on education. Our residents learn from the very beginning which information is relevant and which terminology is correct.
Finally, structured reporting produces digital data that can be seamlessly transferred to other clinical subsystems or used directly for scientific evaluation.
How do you collaborate with other disciplines in your workflow?
We work very closely with our clinical partners – both through the structured reporting format and in tumor boards, of course.
Taking the example of prostate imaging: with mint Lesion, we can now provide urologists with our reports in an optimized format. All lesions are documented with screenshots and schematic drawings, so the information is directly available to our urological colleagues during surgery, for example, in systematic fusion prostate biopsies. This allows lesions to be easily identified and localized again during the ultrasound-guided procedure.
How has using mint Lesion influenced your workflow?
Since implementing mint Lesion, we’ve already seen a noticeable increase in reporting efficiency. The time-consuming manual segmentation of the prostate and the separate documentation of individual lesions with screenshots are now automated by the software.
This has been well received not only by our referring urologists within the hospital but also by our external referrers, who send their patients to us for imaging.
What role does artificial intelligence play in your workflow?
The integrated AI systems significantly support us in segmenting the prostate and suggesting potential lesions as a ‘second reader’. They also help us refine and validate our own subjective lesion assessment.
What trends are you currently observing in prostate diagnostics?
In general, I believe that in the future of oncologic imaging, we will increasingly use AI systems tailored to specific clinical questions.
In prostate imaging specifically, the new S3 guidelines will lead to a considerable increase in MRI examinations – moving toward more non-invasive diagnostics and longitudinal monitoring.
This means: more imaging in less time, potentially without contrast media, but also more reports. Any tool that supports us in documentation is therefore extremely valuable, as it allows us to focus on what truly matters: analyzing the images rather than spending excessive time on documentation.
We thank Prof. Dr. Thorsten Persigehl for sharing his insights and giving us a closer look into the clinical routine of prostate diagnostics. His perspective illustrates how structured reporting and AI are already creating tangible value in radiology today—for radiologists, clinical partners, and patients alike.
Univ.-Prof. Dr. Thorsten Persigehl is Professor of Oncologic Imaging at the University of Cologne and Head of the Radiologic CIO (radCIO) at University Hospital Cologne. Since February 2024, he has served as Associate Editor of Cancer Imaging, the official journal of the International Cancer Imaging Society (ICIS).
Related Resources
Related Resources
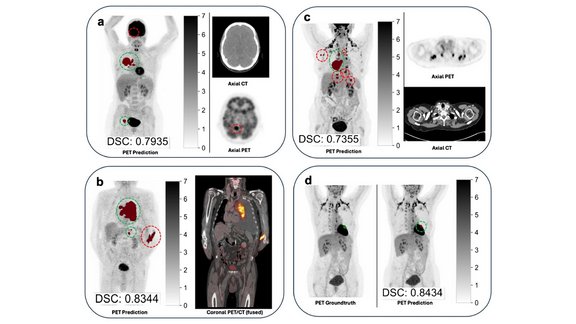
LMU University Hospital: Artificial Intelligence for TNM Staging in NSCLC – How Reliable Are AI-Based Segmentations?
The recent study “Artificial intelligence for TNM staging in NSCLC – a critical appraisal of segmentation utility in [¹⁸F]FDG PET/CT” provides a…

Successful “RECIST and Beyond” Workshop in Cologne: Advancing Precision in Oncologic Imaging
How can complex tumor findings be assessed accurately, reproducibly, and in line with clinical guidelines?

Implementing RANO 2.0 for Neuro-Oncology Clinical Trials in mint Lesion
Tumor response assessment in neuro-oncology clinical trials requires careful attention to measurement protocols and confirmation scan requirements. To…
