Using data from a large cohort of individuals without radiological tumor burden, researchers from University Hospital Cologne have conducted a study [1] aiming at establishing guidance values for absolute iodine concentrations and perfusion ratios of various abdominal organs and lymph nodes, as well as other anatomical landmarks.
Iodinated contrast media are nearly always administered in oncologic computer tomography (CT) imaging, and dual-energy CT (DECT) allows for accurate and reliable quantification of iodine, providing information regarding its distribution. “To pave the road towards clinical application of iodine quantification […] it is pivotal to understand normal distribution and cohort-specific variance of these [iodine] values,” explains PD Dr. Große Hokamp. “However, data on physiological iodine distribution in subjects without tumor burden is sparse.”
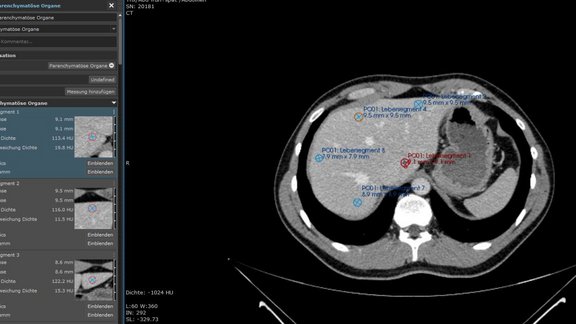
571 portal venous phase dual-layer spectral detector CT studies of the chest and abdomen from patients with no tumor burden confirmed by follow-up imaging after at least three months were assessed. The researchers used mint Lesion™ to place a total of 37 ROI per examination in parenchymatous organs (n = 25), lymph nodes (n= 6), and vessels (n = 3) on conventional images and to copy them to identical positions in iodine maps.
For each ROI, iodine concentration (IC) and its standard deviation were exported. The distribution parameter was calculated to assess the spread of IC and iodine perfusion ratio.
Absolute iodine concentration significantly differed between body mass index (BMI), genders, and age groups in parenchymatous organs, lymph nodes, and vessels (range 0.0 ± 0.0 mg/ml – 6.6 ± 1.3 mg/ml). For instance, higher results were observed for female patients in all ROI (all p ≦0.004). “Hence, care should be taken in providing cutoff values of iodine concentration to differentiate between healthy and malignant abdominal lesions,” the researchers emphasized. “Particularly in studies with a small patient sample, any bias with regard to age and/or sex should be considered and accounted, e. g., in studies with cohorts of higher age, an adaptation to decreased perfusion values should be conducted.”
Widespread differences in iodine perfusion ratios between genders and age groups were recorded in almost all abdominal organs when applying a fixed volume of contrast media. Therefore, the researchers suggest “normalizing absolute iodine concentrations to adjust for the ratio of body weight and applied amount of contrast media.”
This study provides guidance values of IC valid for examinations based on results obtained from a dual-layer SDCT only. “Yet, as different studies showed that iodine quantification can be accurately performed on all different DECT scanners, examinations with a comparable examination protocol can be expected to provide similar results,” the authors pointed out.
Nevertheless, to make quantitative imaging parameters from DECT applicable in clinical settings, international agreement and guidance should be defined by professional societies in cooperation with hardware and software manufacturers – similar to the efforts that have been successfully made by the Quantitative Imaging Biomarkers Alliance and the European Imaging Biomarkers Alliance for different other imaging techniques.
[1] Zopfs, D., Graffe, J., Reimer, R.P., …, Große Hokamp N. Quantitative distribution of iodinated contrast media in body computed tomography: data from a large reference cohort. Eur Radiol (2020), https://doi.org/10.1007/s00330-020-07298-3
University Hospital Cologne: Study provides guidance values of iodine concentration for body CT examinations
Related Resources
Related Resources

Rare Tumors, Big Goals: How RACOON-SAGA Aims to Improve Therapy Decisions
Rare tumors, major challenges: The RACOON-SAGA project explores how imaging and clinical data can improve the pre-therapeutic characterization of soft…

Structured Reporting and Artificial Intelligence in Prostate Diagnostics: An Interview with Prof. Dr. Thorsten Persigehl
What does radiology look like when structured reporting meets artificial intelligence? A look into the daily practice of Prof. Dr. Thorsten Persigehl…

RACOON SAGA: Interdisciplinary Research for Better Therapy Decisions in Sarcoma Treatment
Sarcomas are rare tumors that pose particular challenges to both medicine and research. Their heterogeneity makes precise diagnostics difficult, which…