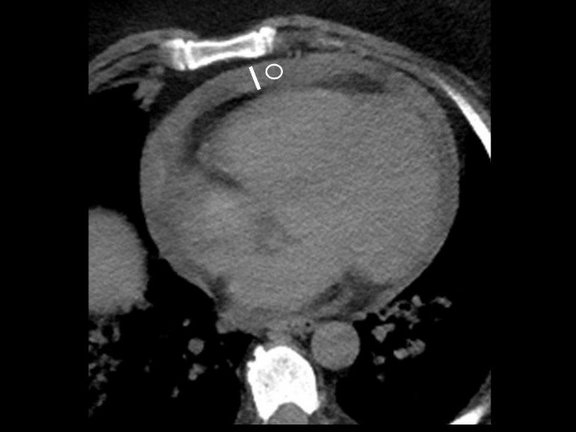
The COVID-19 pandemic wreaked havoc on healthcare systems worldwide, requiring a comprehensive understanding of disease progression for optimal treatment strategies. Amidst this backdrop, the RACOON project of the Netzwerk Universitätsmedizin (NUM) initiated an investigation into the prognostic significance of pericardial effusion (PE) in COVID-19 patients.
Over the years 2019 to 2022, COVID-19 unveiled its diverse clinical spectrum, from mild cases to rapidly progressive, fatal outcomes. As new variants emerged, pandemic preparedness became paramount, urging the need for early prediction of disease progression to optimize patient care. Recognized risk factors for severe outcomes included comorbidities (dementia, heart failure, diabetes), age over 60, male gender, and lung parenchymal involvement.
However, PE's prognostic role remained elusive. While some studies hinted at its significance, contradictions persisted due to limited data and conflicting findings. The present study, a joint effort across 12 university hospitals, aimed to fill this knowledge gap by investigating PE's prognostic relevance in a large, representative cohort.
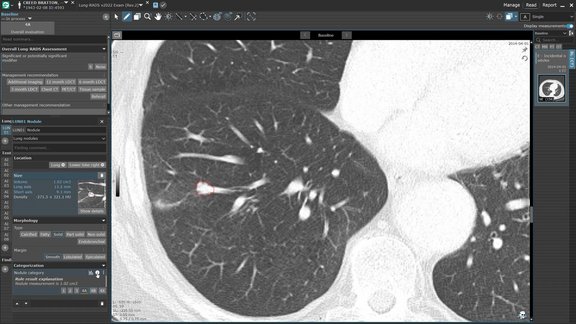
RACOON provided the necessary infrastructure and united the efforts of the participating university hospitals' radiology departments on a single platform. The project uses technology that enables structured acquisition ab initio, i.e., every assessed value is linked with contextual information that defines its clinical significance, thus ensuring traceability, quality, and long-term usability. Moreover, the study accessed a diverse patient pool, ensuring robust data collection and analysis. Thanks to standardized protocols and data curation mechanisms, its retrospective nature didn't compromise its rigor.
PE, often overlooked in COVID-19 assessment, emerged as a critical predictor of 30-day mortality, particularly among male patients. This finding challenged previous notions, suggesting a deeper understanding of the disease's cardiac manifestations. The extensive approach, which analyzed not only the presence of PE but also its breadth and density, expands the comprehension of its prognostic impact.
Furthermore, gender-specific analyses revealed intriguing differences in PE's predictive power, highlighting potential nuances in disease pathogenesis. While the exact mechanisms warrant further exploration, these findings underscored the importance of tailored approaches in patient management.
PE's independence from pulmonary affection suggested its utility as an additional predictor of disease progression. Its inclusion in radiological reports could guide treatment escalation, potentially mitigating adverse outcomes.
Read a summary of this study here.