We all know the phrase “a picture is worth a thousand words”; yet, in specific fields, one thousand words are simply too many and can potentially prove problematic. Radiologists still usually prefer writing reports using prose, often posing hurdles for patient care as a result. Diverse writing styles among radiologists, coupled with varying lengths of text, hedging or typos reduce the overall clarity of a report and impede referring physicians in extracting essential information [1]. For a while now, there has been an attempt at rendering radiology reports more efficient and reproducible by reducing a report’s word count, while increasing precision and homogeneity through the use of structured reporting. The benefits hereof are numerous [1]. For individual radiology workflows, for instance, structured reporting has the potential to minimize time-consuming processes, like queries in form of calls and emails from referring physicians or preparation work for tumor board presentations. For the overall healthcare system, it could result in an overall improvement and uniformity of language enabling interoperability of clinical systems [2] and providing potential benefits for big data analyses [3].
Certainly, structured reporting still has its challenges. It can lead to higher click rates, long click paths, unfamiliar workflows or uncertainties about program usage. Improvements are definitely needed to better align with radiologists’ workflow requirements [4]. The incorporation of artificial intelligence into structured reporting workflows can drive such change forward, but it can also offer potential benefits beyond enhancing radiologists’ efficiency and reducing errors or click rates.
Integrating AI into a framework of structured reporting allows for a different kind of interaction. It accumulates shared knowledge on patient data comprehensible and readable to both, the computer and its user, and it ensures synchronization between the information processed and understood by computers and that understood and delivered by the physicians. Hence, it also fosters improved data accessibility for radiologists and other medical professionals [5; 6]. Lastly, it sets the stage for the implementation and training of additional AI algorithms, leading to a continuous circle of knowledge generation. A long-term vision for this process involves an automated and AI-driven generation of preliminary reports for radiologists to review and supplement with their expert knowledge.
But how do we realize this long-term vision? And how does structured reporting facilitate AI integration and, as a result, improve patient care and big data analysis? Achieving this vision necessitates a gradual process and requires tackling different challenges along the way.
Structured reporting is the linchpin of this journey. To develop sophisticated AI algorithms, we need more extensive training data – data sets that go beyond annotated images and provide more context. “Similar to a developing brain, the development of AI algorithms needs massive amounts of training data, ideally highly specific data, correctly referenced and provided in as structured a form as possible.” [7; see also 8] By presenting information in a consistent manner, structured reports enable AI models to learn patterns and associations and thus serve as valuable training data for AI algorithms [9]. The quantity and quality of data significantly influence the learning and performance of AI algorithms. In healthcare, data often originates from various sources, such as hospitals and clinics – this is where the concept of data liquidity becomes crucial. It enables previously collected data to be used without limitations not only by the ones who collected it but also by other stakeholders, in a different use context and possibly in different systems, while allowing AI algorithms to access a wide variety of patient information.
Structured reports also simplify feature extraction. AI algorithms can extract relevant features from structured reports more effectively compared to unstructured prose reports [10], consequently enhancing a radiologist’s workflow [11]. This advancement could, for instance, eventually lead to patient-friendly multimedia reports containing links to explanations of medical terms [1]. Even further, the combination of “structured radiological reports with other data from electronic health records such as environmental risk factors, genomics, and histopathology” [1] could result in advancements in personalized medicine.
Once again, the key requirement here is to be able to access large amounts of data sets that contain high-quality labels [12], which brings us back to AI training. Extracting relevant information from radiological narrative reports using natural language processing (NLP) is not without errors and may potentially add incorrect labels to a dataset [12], which, depending on the purpose of the AI algorithm, may bear challenges due to related regulatory requirements and quality needs posed towards the training data. The solution thus lies in leveraging the best possible data right from the diagnostic read. Structured reporting templates, such as iRECIST, RADS, and the TNM classification system are instrumental in accurately and comprehensively assessing radiological observations, a crucial step in preparing these findings to train AI algorithms [13]. Current algorithms have commonly not been trained on primary care data but require certified radiologists to annotate existing cases in an additional, secondary read process. Due to the actual medical workflows, building this foundation is presently an arduous task, requiring significant effort, time, and financial resources.
Structured reporting enables radiologists to verify AI findings directly, integrating them seamlessly into their reports. Therefore, we must also ensure that AI can support a radiologist’s workflow to make them more efficient and structured in the first place, for example, by reducing their click rate. This would make structured reporting more efficient and increase its added value. All in all, it is a collaborative effort to create a cycle that can improve the overall process of how a radiological read is being performed and how the radiologist interacts with computer systems.
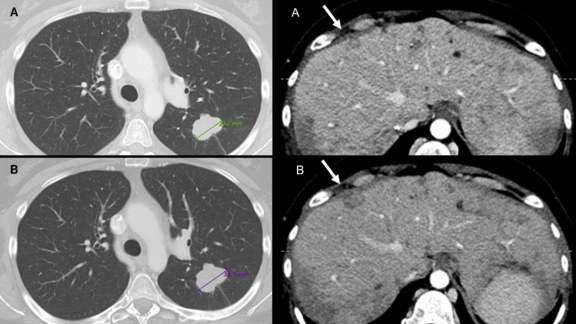
Lastly, the standardized and homogenized language in structured reports facilitate automated data extraction and post-processing [14, 3], significantly reducing manual efforts and potential errors. Currently, in radiology, AI tools are often provided as additional, external systems. Image and clinical data are fed into the tool, which then procures results in form of a static document, such as a PDF. Radiologists can take these results into account while creating their dictated reports. However, AI is not perfect: results can sometimes be faulty or incomplete, requiring critical review and supplementation by the radiologist during their dictation workflow. Direct integration of AI into the structured, image-based reporting process streamlines the use of AI results (as seen with Mint Medical and FUSE-AI in prostate reports, for example). AI results are presented as if processed and prepared by a resident doctor within Mint, complete with measurements and classifications, allowing for immediate confirmation, correction, and supplementation within the system. This integration reduces the currently still existing disconnect between AI systems and radiological reporting, and it is an important step towards the goal of creating a fully reliable, virtual personal assistant.
There are numerous fascinating ideas surrounding the topic of artificial intelligence in medicine, but all in all, artificial intelligence in radiology is here to stay: it “has the potential to add significant value to our care for patients, and to expand the horizons of what imaging can offer” [15]. In order to use this potential, however, a new kind of dialogue needs to happen, in which radiologists and computers maintain a shared understanding of a particular case throughout the read process. Structured reporting is one approach that enables such a dialogue and that assures all data entered or verified by the radiologists being vetted input for subsequent AI assistance in medical device grade products. Hence, an AI-assisted approach to structured reporting can make structured reporting become a part of primary care, enabling radiologists to produce high-quality data accessible for AI training. It is this very ideal that leads us to the long-term vision of computers producing preliminary reports for radiologists to review and supplement with their expert knowledge. So in conclusion, for AI in radiology to keep its promise to improve patient care and quality of life, a picture needs to be worth thousands of structured data points.
At Mint Medical, we understand the nexus of structured radiological data and AI, as well as the opportunities and advantages it presents. A unified lexicon, homogenous language as well as contextual information within reports are the foundation for any future developments in radiology. Together, let us unlock the full potential of data and transform information into actionable insights, thereby contributing to the advancement of healthcare systems. If you want to learn more about the importance of structured reports or mint Lesion™, schedule a demo here.
Sources:
[1] Ganeshan, Dhakshinamoorthy, Phuong-Anh Thi Duong, Linda Probyn et al. 2018 “Structured Reporting in Radiology.” Radiology Research Alliance 25: 66-73.
[2] Christlein, Daniel, Johannes Kast, Matthias Baumhauer. 2021. „Gegenwärtige Entwicklung in der Healthcare-Informationstechnologie: Auswirkungen auf die strukturierte Befundung.“ Radiologie 61: 986-994.
[3] Vosshenrich, Jan, Ivan Nesic, Daniel T. Boll et al. 2023. “Investigating the Impact of Structured Reporting on the Linguistic Standardization of Radiology Reports Through Natural Language Processing Over a 10-Year Period.” Imaging Informatics and Artificial Intelligence 33: 7496-7506.
[4] Jorg, Tobias, Moritz C. Halfmann, Fabian Stoehr et al. 2024. “A Novel Reporting Workflow for Automated Integration of Artificial Intelligence Results Into Structured Radiology Reports.” Insights into Imaging 15.80: 1-10.
[5] McKee, Jennie. 2022. “Responding to ‘Relentless Growth’ of the Radiologist’s Workload.” RSNA, 26 October 2022, www.rsna.org/news/2022/october/workload-and-burnout.
[6] Markotić, Vedra, Tina Pojužina, Dorijan Radančević et al. 2021. “The Radiologist Workload Increase; Where Is the Limit?: Mini Review and Case Study.” Psychiatr Danub 33.4: 768-770.
[7] Pinto dos Santos, Daniel and Bettina Baeßler. 2018. “Big Data, Artificial Intelligence, and Structured Reporting.” European Radiology Experimental 2.42: 1-5.
[8] Filev, Peter D. and Arthur E. Stillman. 2022. “Structured Reporting in Medical Imaging: The Role of Artificial Intelligence.” In: De Cecco, C.N., van Assen, M., Leiner, T. (eds). Artificial Intelligence in Cardiothoracic Imaging: Contemporary Medical Imaging. Humana, Cham.
[9] European Society of Radiology (ESR). 2023. “ESR Paper on Structured Reporting in Radiology—Update 2023.” Insights Imaging 14: 1-8.
[10] Pinto dos Santos, Daniel, Johann-Martin Hempel, Peter Mildenberger. 2019. “Structured Reporting in Clinical Routine.” Fortschritte Röntgenstrahlung 191: 33 – 39.
[11] European Society of Radiology (ESR). 2018. “ESR Paper on Structured Reporting in Radiology.” Insights Imaging 9: 1-7.
[12] Pinto de Santos, Daniel, Sebastian Brodehl, Bettina Baeßler et al. 2019. “Structured Report Data Can Be Used to Develop Deep Learning Algorithms: A Proof of Concept in Ankle Radiographs.” Insights Imaging 10: 93: 1-8.
[13] Fanni, Salvatore Claudio, Michela Gabelloni, Angel Alberich-Bayarri et al. 2022. “Structured Reporting and Artificial Intelligence.” In: Fatehi, M., Pinto dos Santos, D. (eds). Structured Reporting in Radiology: Imaging Informatics for Healthcare Professionals. Springer, Cham.
[14] Fink, Matthias A. 2023. “From Data to Insights: How Natural Language Processing and Structured Reporting Advance Data-Driven Radiology.” European Radiology 33: 7494-7495.
[15] Brady, Adrian P., Bibb Allen, Jaron Chong et al. 2024. “Developing, Purchasing, Implementing and Monitoring AI Tools in Radiology: Practical Considerations; A Multi-Society Statement from the ACR, CAR, ESR, RANZCR & RSNA.” Insights into Imaging 15.16: 1-19.