Next to clinical examination and endoscopy, cross-sectional imaging plays an important role in the diagnosis of head and neck tumors. Moreover, the choice of therapy is guided by the radiological report. We spoke to Prof. Dr. Meinrad Beer, Medical Director of Diagnostic and Interventional Radiology at the University Hospital Ulm, about the particularities of staging head and neck tumors from a radiological standpoint.
What demands does the assessment of ENT-tumors make of radiology?
There can be no generally valid imaging protocol for staging all tumor entities in the head and neck area, considering that the anatomical challenges vary greatly depending on the tumor localization. CT and MRI can complement each other in a useful way due to the difference in displaying tumor characteristics, and we must obtain an overall picture beyond these modalities.
ENT-tumors do not only pose delicate challenges for radiologists, but also for the attending physicians. Surgical procedures of tumor diseases in the head and neck area can lead to onerous disfigurements and loss of function – this makes clearly and unambiguously communicating with our colleagues all the more important.
What are specific challenges in staging head and neck tumors?
The anatomy of the head and neck area is complex, especially the three-dimensional imaging of individual structures. Moreover, the delimitation of neighboring anatomical structures (larynx, pharynx), particularly in regards to CT scans, is not trivial and requires many years of expertise. The degree of delimitation depends on co-factors – such as the BMI (structures are more easily distinguishable from another if the BMI is high). A differentiated classification is needed in order to integrate this into a diagnostic tool.
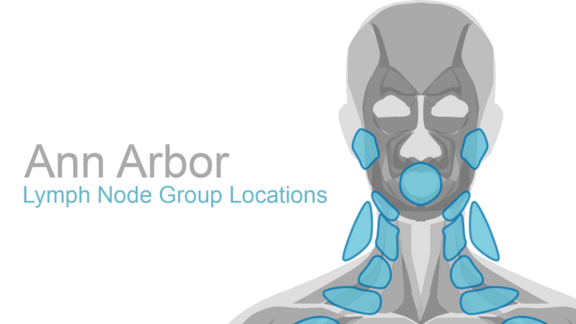
There is also a high number of tumor entities that have to be assessed differently during staging. Synchronous or metachronous secondary tumors – for example in the lung, the esophagus or the colon – are also common. Head and neck carcinomas further have the tendency to develop lymph node metastases rapidly, so the lymph node assessment plays an increasingly important role.
How does mint Lesion™ help overcome these challenges?
Because mint Lesion™ knows all of the rules for assessing the TNM staging for all 12 tumor entities, it systematically guides us through the reporting process. This has definite advantages: Thanks to the clear structure of the results, everything becomes immediately understandable for the referring colleagues. The schematic drawings during the segmentation process in mint Lesion™ even allow peers who are less experienced in imaging ENT-tumors to correctly determine the allocation and delimitation of individual organ structures. Furthermore, the interplay of primary tumor segmentation and lymph node definition facilitates a conclusive and comprehensive staging.
It has now also been recognized that viral infections (such as human papilloma viruses (HPV)) are important etiological factors, too. The current TNM-classification therefore uses the surrogate marker p16 in order to detect the triggering of oropharyngeal carcinomas by HPV. The inclusion of the p16 mutation into the structured reporting of mint Lesion™ represents a trailblazing step towards multimodal, personalized oncological reporting in the head and neck area.