Hepatocellular carcinoma (HCC) is a potentially deadly tumor. The decisive factor is the timing of diagnosis: if HCC is detected early, there is a chance for complete removal and, in the best case, cure. In reality, however, many cases are diagnosed at a late stage, when only intensive and costly therapies remain.
But what if we could change the rules?
This is precisely where the RACOON-MARDER project comes in. MARDER stands for “MRI and AI-assisted personalized HCC risk stratification in chronic liver disease for early intensified screening.” The aim of MARDER is to use MRI data, clinical information, and modern AI approaches to identify those patients at risk who require particularly close surveillance. In this way, a personalized, MRI-based screening strategy could be established that meaningfully complements the currently common, but limited, ultrasound examinations.
In this interview, we speak with Prof. Dr. Timm Denecke, one of the leading minds behind RACOON-MARDER. Prof. Denecke is Professor of Radiology and Chair at Leipzig University as well as Director of the Department of Diagnostic and Interventional Radiology at Leipzig University Hospital. With his expertise in hepatopancreatic imaging, he provides in-depth insights into the aims, challenges, and opportunities of the MARDER project.
Professor Denecke, how did the RACOON-MARDER project come about?
The idea for MARDER arose from discussions about liver projects with my research partners here at Leipzig University Hospital. We are already working on two collaborative projects that both deal with chronic liver diseases and the development of HCC. It is well known that this risk is increased in patients with liver cirrhosis, but it is not evenly distributed. We still do not fully understand in whom and when HCC will develop and which cascade of biological processes leads to it.
In these existing projects, in addition to radiological imaging, we use detailed analyses such as genomics and proteomics in order to model virtual representations of liver tissue damage and malignant transformation to HCC.
In my view, this approach is extremely innovative because it combines finely resolved analyses with radiological imaging at the macro level and thus provides a holistic picture. However, it is based on prospectively collected data in small patient cohorts, because this kind of data collection is very elaborate.
For me personally, that could not be the only path. If I want to arrive at clinically usable results quickly, I do not want to rely solely on prospective data from small patient groups, but rather on data that we already have. Our goal is to develop an instrument in as short a time as possible for the broader population of at-risk patients – a tool that helps to better estimate an individual patient’s HCC risk. And that is where AI comes into play.
From AI research in radiology, we know that such developments are particularly successful when based on retrospective data, provided that sufficiently large amounts of well-referenced data – i.e., where the clinical outcome for the question of interest is already known – are available. This requires extensive, high-quality datasets, including relevant additional clinical parameters. So, we need imaging data from patients we know had later developed HCC. MRI data are the most promising for this purpose. In addition, we need a control group of patients who demonstrably did not develop HCC within a defined time period.
On this basis, an algorithm can then be trained on the MRI scans and clinical data to calculate the risk of developing HCC within a short timeframe, based on the baseline MRI – in other words, to estimate when, where, and in whom liver cancer might arise. In doing so, we adopt the same core idea and structure as the original RACOON project proposal but transfer it to radiological imaging: retrospective, data-driven, and with the goal of achieving a clinically applicable result in a timely manner. It is a very well-suited use case for our NUM-RACOON framework.
Why is it so important to predict hepatocellular carcinoma at an early stage?
Hepatocellular carcinoma is a potentially deadly tumor. The earlier it is detected, the better the chances of completely removing the tumor and, in the best case, curing the patient – similar to breast or prostate cancer, early detection plays a key role here.
However, HCC has a particular feature: unlike breast or prostate cancer, there is no generally elevated (sex-specific) risk in the general population to develop liver cancer. Patients with an increased HCC risk have a damaged liver – a chronic liver disease. At the time of HCC diagnosis, this significantly limits the surgical options for removing the tumor. For small tumors, liver transplantation is an option. It is therefore especially important to detect the tumor early and at a small size in order to preserve as much functional liver parenchyma as possible during therapy and still be able to remove the tumor.
Another crucial aspect concerns liver transplantation. It can remove both the HCC and the underlying liver disease. However, because donor organs are very limited, only patients whose tumors are still small and who have a low risk of tumor recurrence are eligible. Here again, early detection is key to providing a chance of cure.
What are the objectives of the MARDER study and which challenges need to be addressed?
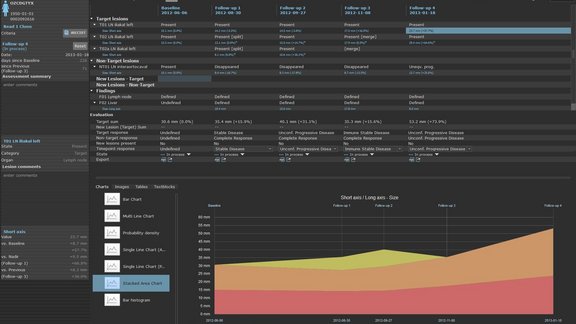
The aim of the MARDER study is not early detection per se, but the development of an instrument for risk stratification. Patients should be assigned to specific risk groups – for example, those with a very high risk of developing HCC within the next three years, and those with a significantly lower risk.
Such high-risk patients are already included in screening programs today. Screening is usually performed using native ultrasound, i.e., B-mode sonography. This is not very sensitive for early detection: the liver is not always fully visualized, and small nodules may remain undetected.
This is where the MARDER study comes in: with precise risk stratification, high-risk patients could be monitored more closely – for example, with more complex and cost-intensive methods such as MRI. For the general population this would not be feasible, but for a smaller subpopulation with proven increased risk, more intensive screening would make medical and economic sense.
How could your research findings improve day-to-day clinical practice and patient care?
If the study is successful, an algorithm could in future calculate the risk of developing HCC – with a percentage probability and a defined time window. High-risk patients could then be included in an intensified surveillance program.
This would mean closer and more precise imaging, as well as greater awareness on the part of patients regarding the importance of follow-up examinations. Today, it is still common that patients miss surveillance appointments and valuable time is lost. A clear risk label would help ensure that such patients do not “slip through the cracks.”
Importantly, no one would receive worse care or be removed from screening. Surveillance would simply be intensified in a targeted way where it promises the greatest benefit. There would therefore be no blanket all-clear, but rather a focused sensitization for those patients in whom it is crucial and who can genuinely gain years of life. But first, of course, we need to do the MARDER work before the screening strategy can be fundamentally reconsidered.
What role does artificial intelligence play in your project?
Even today, certain risk markers can sometimes be identified on MRI scans – for example, dysplastic nodules. Clinical risk factors, such as the cause and extent of the liver disease (e.g., viral etiology or alcohol), also play a role. Clinically and radiologically, we already have tools to adjust risk estimates upward.
Artificial intelligence now adds objectivity to this process. Many patterns remain invisible to the human eye – and this is exactly where AI comes in. Using deep learning methods, we plan to train algorithms to identify patterns that are not visually apparent but are associated with an increased risk. AI “makes the invisible visible” and can extract what is essential to determine a patient’s risk – to see where a malignant process may be developing.
An important component of the MARDER project is the control cohort: patients who we know have undergone MRI and have not developed HCC within five years. It would be of little use to train the network exclusively with positive cases.
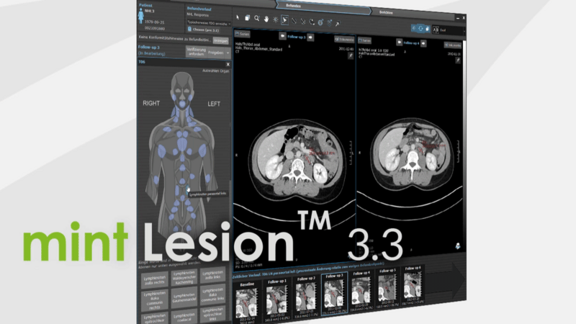
The data basis therefore consists primarily of MRI images, supplemented by clinical information such as the nature and stage of the liver disease and various patient parameters. With such a well-curated dataset, we can drive AI development forward. This also includes smaller sub-goals such as automatic liver segmentation and the identification of the cause and extent of liver disease. Here, we are collaborating with several partners.
Alongside NUM, the core team includes the university hospitals Charité, MHH, LMU, and Leipzig University Hospital. Technology partners such as Fraunhofer MEVIS and Mint Medical as well as developers from DKFZ are also involved. This is an exceptionally strong consortium that is well equipped to meet this challenge.
What further developments do you foresee within the project?
As mentioned, one particularly exciting aspect is that once we have around 800 carefully selected liver MRI studies available, we can use them to address additional questions. For example, developing automated algorithms for the segmentation of organs such as liver, spleen, or pancreas, which are also visualized in MRI.
The goal is to make such methods as robust and device-independent as possible. Currently, MRI scanners deliver very heterogeneous images depending on vendor and sequence, which standard algorithms often cannot handle in a universally reliable way.
In addition, we could further refine the categorization of liver disease using AI: can we automatically infer etiology or disease severity? Can we, for example, estimate the extent of portal hypertension from the data?
These are certainly not “low-hanging fruit,” but ambitious sub-goals. However, this is precisely what makes the project so interesting: intensive work with the data could yield many additional scientific benefits that may later be turned into tools for clinical care.
What role does the RACOON infrastructure play in your project?
We designed the MARDER project specifically as a very well-suited use case for RACOON as it was originally set up. In the first funding phase, with a focus on COVID-19, all German university hospitals contributed lung CT studies.
The process is similar now with MARDER. All university hospitals can contribute suitable cases so that a sufficiently large cohort can be formed to train a reliable algorithm. With currently 38 sites, this would require an average of about 20 cases per site to reach the recruitment target. NUM-RACOON is ideally suited to collect and consolidate imaging and clinical data from across Germany – I am not aware of any comparable network.
The basis of the project is therefore the cases contributed by the sites – and in MARDER, preparation of these cases is particularly demanding. The MRIs do not have to be manually segmented, but the datasets must be carefully selected, precisely referenced, and supplemented with clinical and paraclinical information. It is therefore crucial that as many NUM sites as possible actively participate, contribute cases, and upload data. Only then can we generate a sufficiently large dataset to achieve the project goals.
Beyond the scientific goals: what has your experience been like collaborating with NUM and RACOON?
Within Topic Area 6 of the Network University Medicine (NUM), I have found the collaboration to be extremely constructive and goal-oriented. Many excellent ideas were submitted for the third funding period – far more than could ultimately be funded – and yet the discussions about selection and prioritization were consistently collegial and guided by a higher aim: demonstrating what radiology can contribute within NUM. That was a very positive experience for me. I was impressed by how confidently the radiology community rose to this challenge and how it succeeded in bringing partners from other clinical disciplines and from IT on board.
I particularly welcome the fact that the Federal Ministry of Education and Research (BMBF), which funds NUM, now explicitly requires interdisciplinary collaboration – something I felt was partly missing in the early funding phases. For example, this allowed us to involve hepatology, represented by PD Dr. med. Anna Saborowski from Hannover, in our project, which is essential to stay close to actual clinical needs and to correctly interpret imaging findings in conjunction with paraclinical parameters. Aspects such as gender equity and the integration of multiple sites into the leadership teams of individual projects are now also firmly anchored. That means we truly have to work in a broad network, but it also enables us to obtain first-class input from a wide range of perspectives and areas of expertise.
For me personally, this has been very enriching: these requirements have significantly expanded my own professional network. They foster communication and exchange – and I see that as a key success factor for any project within NUM and Topic Area 6.
The conversation with Prof. Denecke illustrates how crucial interdisciplinary collaboration and structured data collection are for liver research. We thank Prof. Denecke for his valuable insights and wish the project continued success.
RACOON-MARDER is one of seven projects in NUM 3.0 Topic Area 6. In addition to MARDER, BRAIN-AI, COMPARE, INCLUDED, LCS, PAIN, and PROSTAIT are also being funded. The project has a broad foundation: the core team includes, alongside Leipzig University Hospital, Hannover Medical School (with PD Dr. med. Anna Saborowski and Prof. Dr.-Ing. Andrea Schenk), Prof. Dr. med. Dominik Geisel from Charité Berlin, and LMU Munich under the leadership of Prof. Dr. med. Sophia Stöcklein. On the technology side, Fraunhofer MEVIS, the German Cancer Research Center (DKFZ), and Mint Medical provide support.
If you would like to learn more about the ongoing projects, please visit the Network University Medicine (NUM) website or the RACOON Network pages.