The establishment of a nation-wide lung cancer screening program in Germany has been a subject of considerable interest and debate among healthcare professionals, researchers, and policymakers for quite some time. Lung cancer continues to be a major health concern in Germany, affecting thousands of people each year. The recent publication in the Deutsches Ärzteblatt (German Medical Journal) has provided insights into the current status of the nation-wide lung cancer screening program in Germany using low-dose computed tomography (LDCT).
The reason behind the lung screening program
In 2018 lung cancer was the leading cause of death in men (28,365) and the second most common cause of cancer-related death in women (16,514)[1]. The majority of lung cancer cases are linked to smoking tobacco, with estimates suggesting that smoking causes over 60% of all lung cancer cases in women and up to 90% of cases in men. Smokers and former smokers face significantly higher risks of developing lung cancer compared to non-smokers, where male cigarette smokers have up to 24 times higher risk than non-smokers.
Since early-stage lung cancer causes no symptoms, unfortunately, over 70% lung cancer cases in Germany are diagnosed at an advanced stage, which results in poor prognosis. Therefore, early detection is crucial for better outcomes, which potentially can be achieved through a lung cancer screening program with LDCT. Studies have shown that LDCT screening can reduce lung cancer mortality by 15% in high-risk individuals, such as heavy smokers.
Current status of the screening program in Germany and the requirements for its successful implementation
While national lung cancer screening programs have been implemented in the US and are being implemented in Poland, Italy, and Croatia, Germany is yet to follow suit. The potential implementation of such screening program in Germany is currently being explored.
To ensure the successful implementation of the program, certain key aspects need careful consideration. Firstly, it is essential to clearly define the high-risk population that would benefit from screening. Additionally, aspects such as education, the integration of smoking cessation support, and quality assurance for screening and subsequent diagnostic or therapeutic procedures are of paramount importance.
The responsibility of developing concrete implementation recommendations lies with the relevant professional societies. It is imperative to ensure the feasibility of comprehensive recruitment by pulmonologists and to retain the target population within the program. With approximately six million people at risk, a comprehensive and well-supported national program with proper infrastructure and budget is essential.
In addition, there is a need to address challenges related to false-positive findings, potential overdiagnosis, and the balance between the benefits of screening and radiation risks. Two ongoing studies, namely the Hanse study and the European 4-IN-The-Lung-RUN study, are providing valuable insights to guide the development and implementation of a quality-assured lung cancer screening program in the country.
According to Prof. Dr. med. Maria-Katharina Ganten, a renowned radiologist who have participated in the German LUSI study (German Cancer Research Center) as well as the ongoing British NHS Targeted Screening for Lung Cancer with LRDCT, the success of the lung screening initiative in Germany hinges upon harnessing the potential of advanced technologies.
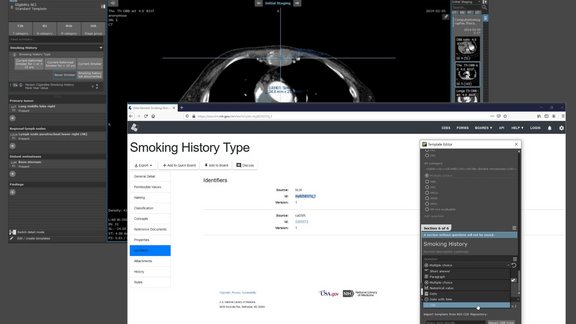
“For systematic analyses of data and the effective support of screening initiatives, the integration of AI-solutions and computer-aided detection becomes crucial. These advanced technological tools can play a transformative role in enhancing the accuracy and efficiency of early detection measures for lung cancer among high-risk individuals. Moreover, the establishment of standardized data collection and aggregation, such as in clinical registries, would further reinforce the screening process, facilitating comprehensive and systematic data analysis,” says Prof. Ganten.
As the lung screening initiative advances, continued research and development in computer-aided lung nodule detection, structured reporting and standardized data collection will undoubtedly refine and optimize the screening process further. By adopting a proactive and technology-driven approach, Germany has the opportunity to develop a comprehensive and cutting-edge lung screening program. This would represent a significant step forward in reducing the burden of lung cancer and improving the health outcomes for individuals at risk.
More about the background and the current status of the lung screening program in Germany can be found here (in German).
[1] Reck, M., Dettmer, S., Kauczor, H. U., Kaaks, R., Reinmuth, N., & Vogel-Claussen, J. Lungenkrebs-Screening mittels Niedrigdosis-Computertomografie: Aktueller Stand in Deutschland. Dtsch Ärzteebl Int 2023; 120: 387-92 ; DOI: 10.3238/arztebl.m2023.0099